The Evidence Behind Evidence-Based LeadershipSM
By: Lynne Mahony, MBA, MFA, Matthew Bates, MHA, Stephanie Striepeck, MBA
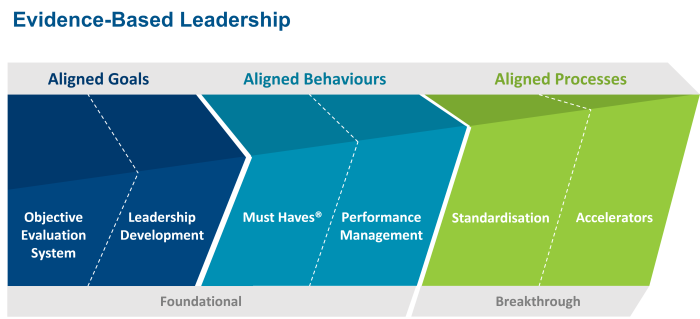
Studer Group’s Evidence-Based LeadershipSM Operating Framework
An analysis of the Hardwiring Excellence framework (the predecessor to EBL) identified numerous empirically grounded theoretical underpinnings to its principles, including motivation and feedback, management by objectives, evidence-based management, and organizational learning. Further, its effectiveness in driving quality outcomes in healthcare is comparable to other evidence-based models such as Lean/Six Sigma and Baldrige.i
“Our review of the Nine Principles®, pillars, and Must Haves® of the Studer approach found this framework to be closely aligned with management-related concepts of motivation and feedback, social networks, human capital, social capital, management by objectives, evidence-based management, and organisational learning. The dynamics set in motion by these elements of the Studer approach are major changes in behavior, attitudes, relationships, processes, and goal attainment that hardwire excellence.”ii
Leadership is the single most important variable when implementing Evidence-Based LeadershipSM,iii but absorbing the initiative into an organisation’s culture is the key to sustainability.iv
Objective Evaluation System
Objective evaluation systems that include employee participation in goal setting and continual feedback about results are associated with improved performance quantity, improved performance quality, and increased employee satisfaction with leadership.v
Organisations who successfully close the strategy-to- performance gap make goals concrete, identify fewer, but clear priorities, continuously monitor performance, and reward execution capabilities.vi
Leader Development
Companies with effective leader development are more effective at driving improved business results through leadership skill, and effective leadership development programs foster organisational agility during change.
Leadership development not only develops leaders, but creates a culture of performance. Leadership development for internal staff is more effective than hiring externally.
Must Haves®
Note: The Must Haves® for Studer Group’s work with partner organisations may vary based on the type of organisation and their priorities. However, the following evidence-based behaviours represent the Must Haves® relevant at most hospitals.
ROUNDING
Leader Rounding on Employees: Leader rounding on employees reduces turnover viii and promotes safety.ix
Leader Rounding on Patients: When leaders round on patients, the patient’s perception of the care received is not only improved, but the clinician also rates the quality of care provided as higher.xi
Leader Rounding on Internal Customers: Satisfaction with internal service quality is more powerful than satisfaction with wages and benefits in predicting job satisfaction.xii
Senior Leader Rounding: Senior leader rounding promotes employee engagement and increased patient experience through increased communication and executive visibility.xiii
THANK YOU NOTES/REWARD AND RECOGNITIONxiv
Reward and recognition (tangible or non-tangible) has positive effects on employee commitment and motivation and stimulates creative performance. Lack of recognition is a crucial reason for employee turnover. Employees do their best work when they feel that their hard work will be rewarded by their manager.
KEY WORDS AT KEY TIMES/AIDET®
Using communication that involves the patient in their care establishes better rapport, which is associated with improved clinical outcomes and self-management of health conditionsxv, increased patient satisfaction, and decreased malpractice claims.xvi
EMPLOYEE SELECTION
Peer interviewing increases new employee retention as well as helping with the transition of employees into their new roles and empowering peer interviewers to aid in the selection of new team members.xvii
Effective onboarding of new employees results in improved retention, time to productivity, job satisfaction, and customer satisfaction.xviii
PRE- AND POST-VISIT CALLS
Pre-visit phone calls reduce the rate of no-shows.xix
Post-visit phone calls increase patient experience, reduce adverse events (including readmission and death), and increase staff morale and empowerment.xx
Performance Management
Unaddressed disruptive behaviour leads to higher healthcare expenses, risk of malpractice litigation, and decreased staff morale as well as increased turnover and job dissatisfaction.xxi
Effective performance management (with every employee receiving at least an annual performance review) leads to stronger financial performance, achievement across all organisational goals, and organisational growth.xxii
Standardisation
Standardisation maximises adherence to evidence-based processes of care and results in improved clinical outcomes, shorter hospital stays xxiii, reduced malpractice litigation xxiv, and improved patient safety.xxv
Highly reliable organisations focus on sets of standardised principles that enable them to focus attention on emergent problems and deploy the appropriate resources to address those problems. They foster a culture that celebrates failures as “windows into the health of the system, they seek out problems, they avoid focusing on just one aspect of work and are able to see how all the parts of work fit together, they expect unexpected events and develop the capability to manage them, and they defer decision making to local frontline experts who are empowered to solve problems.”xxvi
Accelerators
Information technology (IT) is associated with substantial increases in output and productivity; organisations that implement IT are also likely to implement new business processes, new skills, and new organisational and industry structures. Greater levels of IT are associated with increased delegation of authority to individuals and teams and greater levels of skill and education in the workforce.xxvii
A technology-enabled performance management tool [like Studer Group’s Leader Evaluation Manager®] encourages managers to develop better ongoing performance management behaviours, xxviii increases the effectiveness of performance feedback, xxix and is critical not just for business intelligence, but also as an analytical online process, a data warehouse and a simulation tool.xxx

References:
i Robbins, J., Garman, A., Song, P., McAlearney A.S. (2012). How High-Performance Work Systems Drive Health Care Value: An Examination of Leading Process Improvement Strategies. Q Manage Health Care, 21(3): 188-202.
ii Spaulding, A.C., Gamm, L.D., Griffith, J. M. (2010). Studer Unplugged: Identifying Underlying Managerial Concepts. Hospital Topics, 88(10: 1-9.
iii Schuller, K.A., Kash, B.A., Edwardson, N., & L.D. Gamm. (2013). Enabling and disabling factors in implementation of Studer Group’s Evidence-Based Leadership initiative: A qualitative case study. Journal of Communication in Healthcare, 6(2), pages 90- 99.
iv Schuller, K. A., Kash, B. A., Gamm, L. D. (2015) Studer Group’s Evidence-Based Leadership Initiatives. Journal of Health Organization and Management, 29(6): 684-700.
v Thompson, K.R., Luthans, F., & W.D. Terpening. (1981). The effects of MBO on performance and satisfaction in a public sector organization. Journal of Management, 7(1), pages 53-68. Full text retrieved from http://digitalcommons.unl.edu/cgi/viewcontent.cgi?article=1021&context=leadershipfacpub on 12/1/15.
vi Mankis, M., & Steele, R. (2005). Turning Great Strategy into Great Performance. Harvard Business Review, 7. Retrieved from https://hbr.org/2005/07/turning-great-strategy-into- great-performance on 8/18/16.
vii Martineau, J., Hoole, E., Patterson, T. (2009). Leadership Development: Is It Worth the Money? Management Development. EFMD Global Focus 93(03): 44-47. http://www.ccl.org/ leadership/pdf/news/EFMD09LeadershipDevelopment.pdf.
viii Hinson, T.D., & D.L. Spatz. (2011). Improving nurse retention in a large tertiary acute-care hospital. Journal of Nursing Administration, 14(3), pages 103-108.
ix Frankel, A., Grillo, S.P., Pittman, M., Thomas, E.J., Horowitz, L., Page, M., & B. Sexton. (2008). Revealing and resolving patient safety defects: The impact of leadership WalkRounds on frontline caregiver assessments of patient safety. Health Services Research, 43(6), pages 2050-2066.
x Kennedy, B., Crag, J.B., Wetsel, M., Reimels, E., & J. Wright. (2013). Three nursing interventions’ impact on HCAHPS scores. Journal of Nursing Care Quality, 28(4), pages 327-334.
xi McIntosh, N., Burgess, J.F. Jr., Meterko, M., Restuccia, J.D., Alt-White, A.C., Kaboli, P., & M. Charns. (2014). Impact of provider coordination on nurse and physician perceptions of patient care quality. Journal of Nursing Care Quality, 29(3), pages 269-279.
xii Hallowell, R., Leonard A.S., & J. Zornitsky. (1996). Internal service quality, customer and job satisfaction: Linkages and implications for management. Human Resource Planning, retrieved from http://edtech2.tennessee.edu/projects/USDA/isq.pdf on 11/17/15.
xiii Executive rounding program improves communication, performance (2006). Performance Improvement Advisor, 10(8), 94-6.
xiv Gohari, P., Kamkar, A., Hosseinipour, S.J., & M. Zohoori. (2013). Relationship between rewards and employee performance: A mediating role of job satisfaction. Interdisciplinary Journal of Contemporary Research in Business, 5(3), pages 571-597.
xv Heisler, M., Bouknight, R. R., Hayward, R. A., Smith, D. M., & Kerr, E. A. (2002). The relative importance of physician communication, participatory decision-making, and patient understanding in diabetes self-management. Journal of General Internal Medicine, 17, 243-252
xvi Huntington, B., & Kuhn, N. (2003). Communication gaffes: A root cause of malpractice claims. Baylor University Medical Center Proceedings, 16, 157-161
xvii Crawford, L. (2011). Using Peer Interviewing to Reduce Nursing Turnover and Vacancy and Improve Staff Satisfaction. Emergency Nurses Association. Presentation. Retrieved from: http://www.nursinglibrary.org/vhl/handle/10755/162424
xviii Bauer, T.N. (2010). Onboarding new employees: Maximizing success. SHRM Foundation, retrieved from https://www.shrm.org/about/foundation/products/Documents/ Onboarding%20EPG-%20FINAL.pdf on 11/13/15.
xix Christensen, A.A., Lugo, R.A., & D.K. Yamashiro. (2001). The effect of confirmation calls on appointment-keeping behavior of patients in a children’s hospital dental clinic. Journal of Pediatric Dentistry, 23(6), pages 495-498.
xx Kennedy, B., Crag, J.B., Wetsel, M., Reimels, E., & J. Wright. (2013). Three nursing interventions’ impact on HCAHPS scores. Journal of Nursing Care Quality, 28(4), pages 327-334.
xii Reither, C.E., Pichert, J.W., & Hickson, G.B. (2012). Addressing behavior and performance issues that threaten quality and patient safety: what your attorneys want you to know. Progress in Pediatric Cardiology, (33)1, pages 37-45.
xxii “How Smart HCM Drives Financial Performance,” Workforce Intelligence Institute & SuccessFactors, 2006.
xxiii Bozic, K.J. et al. (2010). The influence of procedure volumes and standardization of care on quality and efficiency in total joint replacement surgery. Journal of Bone and Joint Surgery, 92(16), pages 2643-2652.
xxiv Kirkpatrick, D.H. & R.T. Burkman. (2010). Does standardization of care through clinical guidelines improve outcomes and reduce medical liability? American Journal of Obstetrics & Gynecology, 116(5), pages 1022-1026
xxv Rozich, J.D. et al. (2004). Standardization as a mechanism to improve safety in health care. The Joint Commission Journal on Quality and Patient Safety, 30(1), pages 4-14.
xxvii Christianson, M.K., Sutcliffe, K.M., Miller, M.A., & Iwashyna, T.J. (2011), Becoming a high reliability organization. Critical Care, 15(6), 314.
xxvii Brynjolfsson, E. & L.M. Hitt. (2000). Beyond computation: Information technology, organizational transformation, and business performance. Journal of Economic Perspectives, 14(4), 23-48.
xxviii Hunt, S. T. (2011). Technology is transforming the nature of performance management. Industrial and Organizational Psychology, 4(02), 188-189.
xxix Gueutal, H., & Stone, D. L. (2003). The brave new world of e-HR. Advances in human Performance and Cognitive Engineering Research, 3, 13-36.
xxx Smith, M. A., & Kavanagh, S. C. (2008). The Potholes of Performance Management Technology: A New Road and Its Obstacles. Government Finance Review, 24(3), 63-66.